Supply chain problems and poor quality or counterfeit drug manufacturing - in combination with restrictions on opioids - limit access to pain medications in low- and middle-income countries (LMICs). In particular, rural regions often have minimal, inadequate or no drugs available. A variety of traditional remedies are also used.
Aspirin and Paracetamol
Paracetamol:

Photo courtesy of Ambrose
Heron, Creative Commons
In low-resource settings, aspirin and paracetamol are among the most widely available medicines. The WHO recommends aspirin (acetylsalicylic acid) and paracetamol (acetaminophen) for the relief of mild-to-moderate pain. Aspirin is believed to be the most commonly used analgesic medication worldwide with 40,000 metric tons consumed each year. Similarly, paracetamol, which was first used clinically in 1893, relieves pain and fever.
Ketamine
Ketamine:

Photo courtesy of the U.S.
Drug Enforcement Agency
Since 1985, the WHO has included ketamine on its essential medicine list to relieve pain and provide anesthesia for both children and adults. Discovered in 1962, this dissociative anesthetic is either injected into a muscle or given intravenously - administering the drug, then, does not require reliable electricity, oxygen, highly trained staff or monitoring systems. In comparison to other anesthetics, ketamine does not depress breathing or lower blood pressure. This combination of ease of use and high level of safety means ketamine can be used to reduce pain during surgical procedures in LMICs, disaster situations and conflict zones. For several decades, there have been reports of illicit use of ketamine on a relatively small global scale.
Morphine
Morphine pills:

Photo courtesy of FDA
Opioid analgesics are listed among the WHO essential medicines. Opiates are made from the raw materials of opium, poppy straw and concentrate of poppy straw. Since the earliest human civilization, opium has been known to relieve pain. Morphine, a powerful opium derivative first synthesized in the early 19th century, comes in the form of a bitter-tasting pill or solution. Another form of liquid morphine can be injected into the muscle. In many LMICs, there is limited availability of oral morphine and too few staff trained in palliative care.
Tramadol
Tramadol:
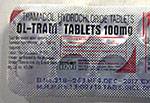
Photo courtesy of FDA
Tramadol, synthesized in 1962, is available globally in tablet, capsule or injectable solution. Tramadol produces dual-analgesic effects. It both activates opioid receptors in the brain, which relieves pain, while also blocking serotonin and noradrenaline absorption in the brain thus affecting mood. Tramadol is used worldwide and is included as an analgesic in the WHO guidelines for cancer pain relief. Tramadol is generally considered a medicinal drug with a low potential for dependence relative to morphine, yet the UN warned of an increase in trafficking and consumption of tramadol at the end of 2017.
Traditional remedies
Acupuncture:

Photo courtesy of the
NIH/NCCIH
Traditional health care encompasses a wide variety of pain-relief remedies. The WHO reports that acupuncture is the most common traditional practice, closely followed by herbal medicines and indigenous traditional medicine. Other popular forms include homeopathy, therapeutic massage, hypnotherapy, hands-on healing and hydrotherapy. More than 100 countries embrace Chinese traditional medicine, with some people using it exclusively and others as a complement to allopathic medicine, according to the WHO.
For pain relief, two techniques, acupuncture and tai chi, as well as herbal remedies are often used within this tradition dating back thousands of years. Practitioners of acupuncture stimulate specific points on the body by inserting thin needles through the skin. Research suggests this ancient technique promotes the release of the body’s natural painkillers and affects areas in the brain involved in processing pain. Past studies reveal that acupuncture can ease certain chronic types of pain, such as low-back pain, neck pain, osteoarthritis/knee pain and carpal tunnel syndrome. Other research shows it may reduce the frequency of tension headaches and prevent migraine headaches. However, some scientific studies suggest that real and sham acupuncture are equally effective, indicating a placebo effect, according to the National Center for Complementary and Integrative Health (NCCIH). Tai chi and yoga combine certain postures, gentle movements, mental focus, breathing and relaxation. Research suggests that practicing tai chi may reduce pain from knee osteoarthritis and help people cope with fibromyalgia and back pain.
Betel nut
Betel nut:

Photo courtesy of the
NIH/NIDA
The betel nut, which is cultivated from the tall, slender Areca palm tree, has been used in the Pacific islands for as many as 2,000 years. An estimated 600 million people take some form of the betel nut to achieve stress reduction, a feeling of well-being and heightened awareness, according to the WHO. A staple of traditional Ayurvedic medicine, the nut is offered to patients as relief for a range of ailments, though evidence of health benefits is limited at best. However, a 2015 study suggested that a treatment made of a betel nut extract conferred significant pain reduction in a rat model of migraine headaches.
Cannabis
Cannabis:

Photo courtesy of the U.S.
Drug Enforcement Agency
About 147 million people consume cannabis, which originated in Central Asia and is now cultivated across the globe, according to the WHO. Cannabis refers to the dried leaves, flowers, stems and seeds from the
Cannabis sativa or
Cannabis indica plant, which contains the mind-altering chemical THC and similar compounds. For thousands of years cannabis has been used for medicinal purposes, including as an analgesic. Evidence suggests long-term cannabis users risk impairment of cognitive functioning and dependence, while those who smoke it may also damage their airways, inflame their lungs and weaken their defense against pulmonary infections. The NIH’s National Cancer Institute (NCI) states that pain relief is a potential benefit of medicinal cannabis, while various studies suggest patients using cannabis require less frequent and lower doses of opioids. Currently, scientists supported by the NIH are looking at cannabis use to alleviate HIV- and sickle cell disease-related pain.
Khat
Khat:

Photo courtesy of the U.S.
Drug Enforcement Agency
The khat plant (Catha edulis) is cultivated in countries bordering the Red Sea, along the east coast of Africa and in west Asia. For centuries people in these regions have used khat for its stimulant effects and as part of their cultural and religious traditions, according to the WHO. Some khat chewers believe the plant is beneficial for ailments including headaches, colds, body pains, fevers and arthritis. The leaves release chemicals, structurally related to amphetamines, that deliver a mild high. Yet there are a variety of health problems associated with khat, including hypertension, anorexia, constipation, cardiovascular disease, hepatitis and cancer. A 2017 study indicated khat extract is analgesic in mice exposed to different painful stimuli. The authors call for additional explorations of the plant’s effects on pain receptors.