Resistance in the context of ancient & modern diseases
May / June 2022 | Volume 21 Number 3
HIV and Tuberculosis are both very prone to developing antimicrobial resistance, yet they adopt opposite strategies for doing so, said Dr. Patrick Cudahy. The virus that causes AIDS makes a “billion” copies of itself yet the vast majority of them don't work. “But a few of them might actually be impervious to treatment and that's how HIV drives resistance,” said the Yale School of Medicine instructor. By contrast, TB doesn’t mutate much and instead “just hunkers down, waits you out, and takes six months to treat, which is very unique for a bacterial infection,” said Cudahy. In that time, TB seizes every opportunity —inappropriate medication or missed doses of medication—to grow resilient.
Cudahy’s earliest medical training in South Africa took place in “big open wards of TB patients.” Many patients were co-infected with HIV and some undoubtedly had multidrug-resistant tuberculosis (MDR-TB). Even experienced doctors found it difficult to measure treatment response. “That’s how I got interested in developing a biomarker—a very early signal—that can tell us if a patient with MDR-TB is responding to therapy,” said Cudahy, describing his
Fogarty-funded project. Study results will help reduce development of new resistance and further transmission of TB by ensuring that patients are on effective medications.
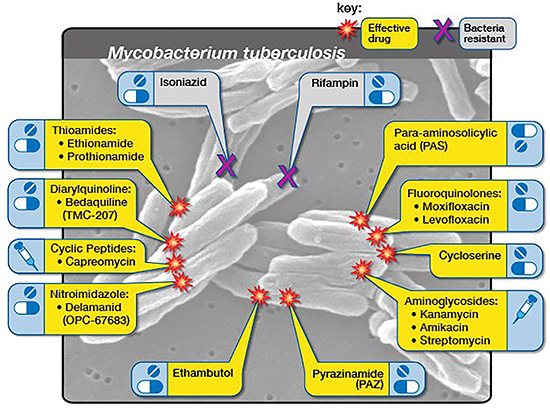 Illustration courtesy of NIAIDMDR-TB occurs when a tuberculosis strain is resistant to first-line drugs. To cure MDR-TB, healthcare providers must turn to a combination of second-line drugs, which may cost 100 times more than first-line therapy.
Illustration courtesy of NIAIDMDR-TB occurs when a tuberculosis strain is resistant to first-line drugs. To cure MDR-TB, healthcare providers must turn to a combination of second-line drugs, which may cost 100 times more than first-line therapy.
TB research represents a departure, of sorts, for Cudahy who first came to South Africa in 2007 to work on HIV. Soon he discovered TB was “much more challenging.” HIV had a blood test for diagnosis and a straightforward, if lifelong, regimen of medications. “To even diagnose TB was difficult and the medications had lots of side effects,” said Cudahy. The good news is nearly 95% of patients with drug sensitive TB, even if they have HIV, can be cured.
The odds are not so favorable for the other 5% of TB patients in South Africa, those with drug-resistant TB. About a quarter of patients with MDR-TB and HIV do not survive. “If a person is exposed to drug-resistant TB—or develops resistance due to being given the wrong drugs or being unable to take their drugs reliably—then they need second line medications,” said Cudahy. Until very recently this meant several pills and daily injections for up to two years with drugs that had “profound” side effects—deafness and kidney injury. “The new WHO drug regimen for MDR-TB is four oral drugs for six months—so that's fantastic progress,” he said. Meanwhile, a new genetic test can detect “the vast majority of MDR-TB. That’s a game-changer since we now know what we're dealing with from the beginning.”
Characterizing epidemic spread
Dr. Karen Jacobson trained in Cape Town, South Africa, not long after scientists had first sequenced the TB genome and begun to recognize mutations predicting resistance to first line drugs (isoniazid, rifapentine, and rifampin). “As sequencing became a standard part of diagnostics, I wondered: Could we use this routinely collected data to better understand disease spread and evolution of disease?”
Her project, funded by Fogarty and completed in 2017 identified regions of the Western Cape Province with a high burden of drug resistant TB. “Even after adjusting for TB burden, we found communities differentially impacted—not every community with a lot of TB also had a lot of MDR-TB.”
The social context allowing TB to spread is well-known, said Jacobson, who is an associate professor at Boston University School of Medicine. Overcrowding, malnutrition, and poverty all contribute to its prevalence. But understanding rifampin-resistant TB is another question. “We’ve come to see in South Africa, which is a more mature epidemic, that most of the resistant TB is actually transmitted. People catch it in that form,” said Jacobson. With the newest diagnostics, doctors can prescribe the correct drug regimen faster and so break the chain of transmission. “But there still are a lot of questions about why in certain communities the rifampin resistance can become so successful,” said Jacobson. One hypothesis is that people with HIV may serve as incubators for resistance evolution resulting in a strain capable of transmitting in the community.
While she continues to work on translating data into a better understanding of disease spread and evolution, Jacobson is “holding my breath to see what happens after COVID-19.” A decline in cases occurred during the last two years, a time when many people avoided clinics, so a TB resurgence may be on the horizon. To prevent spread of MDR-TB, funding and support of ongoing sequencing and early detection of cases is needed. “If resistance to the newer drugs begins, then we need to ask: Where is this occurring? Under what circumstances? Can we add other drugs to the regimen?” said Jacobson. “Tuberculosis, although an ancient disease, is one that’s really been understudied and underfunded. Yet it remains a leading killer globally.”
More Information
Updated June 15, 2022
To view Adobe PDF files,
download current, free accessible plug-ins from Adobe's website.
Related Fogarty Programs
Related World Regions / Countries
Related Global Health Research Topics