Examining the impact of COVID-19 on mortality in the U.S.
November/December 2023 | Volume 22 Number 6
Senior author Cécile Viboud and her colleagues examined the impacts of the COVID-19 pandemic on U.S. mortality in this
eLife study.
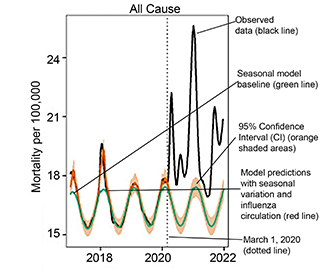 Image adapted from Figure 2 of "Direct and indirect mortality impacts of the COVID-19 pandemic in the United States, March 1, 2020 to January 1, 2022." Courtesy Wha-Eum Lee, et al.The authors estimate there were 102,800 excess deaths from external causes from March 1, 2020, to January 1, 2022.
Image adapted from Figure 2 of "Direct and indirect mortality impacts of the COVID-19 pandemic in the United States, March 1, 2020 to January 1, 2022." Courtesy Wha-Eum Lee, et al.The authors estimate there were 102,800 excess deaths from external causes from March 1, 2020, to January 1, 2022.
At the end of January 2023, Johns Hopkins University reported 1,056,000 total U.S. deaths due to COVID-19, yet some scientists suggest this figure is not high enough. Excess mortality methodologies, which measure increases in mortality over a historical baseline, have been used for more than a century to capture the full scope of infectious disease events as well as of heatwaves and earthquakes. Here, Viboud and her co-authors aimed to disentangle direct and indirect mortality impacts of the pandemic in the U.S. by using regression models and synchronicity analyses.
“Direct effects" of COVID-19, the authors explain, are those deaths that result from SARS-CoV-2 infection and its complications as well as those deaths sparked by viral infection. For instance, a rise in diabetes mortality would be expected to coincide with a rise in COVID-19 cases because some diabetic patients would have died due to an undetected SARS-CoV-2 infection triggering their condition—just as every year deaths from chronic conditions rise alongside seasonal flu deaths.
"Indirect effects," on the other hand, are both the positive and negative changes in mortality that are not linked to an actual SARS-CoV-2 infection during the pandemic period. Possible reasons for these changes include avoidance of health care systems, stressed health care systems, mental health issues in families of severely affected COVID-19 patients, societal disruptions, decreased social interaction that suppresses circulation of endemic pathogens, and decreased air pollution. Indirect pandemic impacts on mental health, violence, and addiction remain debated, especially since these potentially large effects on mortality may or may not coincide (timewise) with COVID-19 waves.
In the U.S., the trajectory and experience of the COVID-19 pandemic varied greatly depending on the region and time period. There were also inconsistencies in the strength and types of interventions implemented in each region. These differences provide an opportunity to separate the contributions of viral infection from other drivers of mortality. To separate direct consequences of SARS-CoV-2 infection on age-specific, state-specific and cause-specific mortality from indirect consequences associated with hospital strain and interventions, the authors applied time series analytic approaches to four large waves of COVID-19 from March 1, 2020, to January 1, 2022.
The pandemic's direct and indirect effects varied substantially by chronic condition and age group, the authors estimated. Somewhere in the range of 65% to 94% of the rise in all-cause mortality could be statistically linked to SARS-CoV-2 activity. This includes the direct contribution of SARS-CoV-2 infection to mortality caused by several chronic conditions, including Alzheimer's, diabetes, and heart disease. Mortality in children and young adults, and mortality from accidents, injuries, drug overdoses, assaults, and homicides, showed a marked relationship with COVID-19 interventions, supporting the idea that indirect pandemic effects (unrelated to an actual SARS-CoV-2 infection) increased death rates. By contrast, cancer and suicides remained within baseline levels. The authors' most striking finding is an estimated 112,200 excess deaths in individuals 25 to 44 years old by January 1, 2022—of these not even a third are ascribed to COVID-19 in the official statistics.
Updated December 11, 2023
To view Adobe PDF files,
download current, free accessible plug-ins from Adobe's website.
Related World Regions / Countries