Facing the challenge of undiagnosed diabetes in Africa
May/June 2023 | Volume 22 Number 3
By Susan Scutti
Sub-Saharan Africa has the highest percentage of people living with undiagnosed type 2 diabetes in the world, according to the
International Diabetes Federation (IDF). An estimated 54% of Africans who are living with diabetes do not know they have the illness, which is characterized by poor regulation of blood glucose (sugar) that is used by the body’s cells for energy. Too much circulating glucose leads to diabetes and its possible complications, including heart disease, renal failure, blindness, neuropathy and lower extremity amputations.
Diagnosing diabetes in Africa is problematic due to costs and lack of access to resources. Additionally, Africans may have a different phenotype of the disease—type 2 diabetes is common in non-obese Africans—which leads to atypical biomarkers and diverging diagnostic standards. Dr. Jean de Dieu Gatete described a new strategy for diagnosing the disease, which could be of specific value to Africa, in his recent graduation speech.
Gatete is the seventh fellow in the
NIMHD-NIDDK-Rwandan Health Program, led by Dr. Anne E. Sumner of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). It is anticipated that Gatete, who is scheduled to return to Rwanda in July 2023, could conduct similar research there, ultimately changing the trajectory, severity and prevalence of undiagnosed diabetes in the sub-Saharan Africa nation.
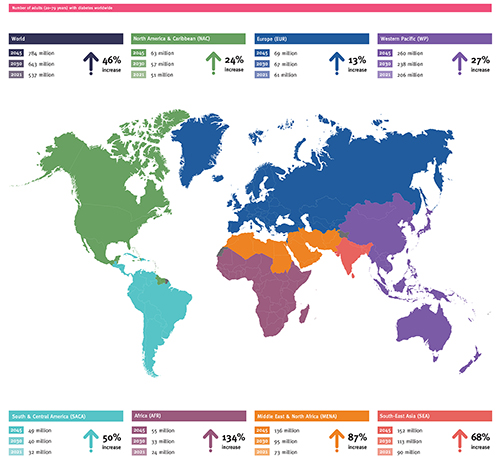 Image courtesy of RAFTI-USA While the International Diabetes Federation projects a 46% increase in diabetes worldwide over the next two decades, it expects prevalence in Africa to increase by 134%.
High-resolution image JPG, 612KB]
Image courtesy of RAFTI-USA While the International Diabetes Federation projects a 46% increase in diabetes worldwide over the next two decades, it expects prevalence in Africa to increase by 134%.
High-resolution image JPG, 612KB]
Accessible, inexpensive solution
The best, most reliable test for diabetes, the oral glucose tolerance test (OGTT), measures how the body reacts to a solution with high glucose content called “glucola,” explained Gatete. It begins with a blood draw from a patient who’s fasted for eight hours, followed by measurement of blood glucose levels; after the patient drinks glucola, another blood draw takes place two hours later to check glucose levels. When high levels of blood sugar are seen, the patient has diabetes (or, if levels are not so high, pre-diabetes). Glucola, which is rarely available on the continent, costs $8 a bottle, prohibitively expensive in many places in sub-Saharan Africa according to Gatete.
Seeking a glucola alternative, the NIMHD-NIDDK-Rwandan Health team first tried substituting Ceres Juice, a South African brand, but found it did not identically affect blood glucose levels so could not be used for diagnosis. Next, the team mixed water and pastry sugar (also known as confectioner’s or powdered sugar) and found a solid match to the performance of glucola. Add the cost of the sugar needed for the test is less than a dollar.
To validate this work, a pastry sugar tolerance test (PSTT), which enrolls African immigrants in the U.S., is underway, said Gatete. The plan is for Gatete and others to conduct the same research in Africa. For Rwanda, a nation similar in size to the state of Maryland with a population of 14 million, the use of PSTT as a diabetes diagnostic should be within economic reach.
Tackling a disease triumvirate
Gatete also proposed a “provocative theory” that diabetes should be considered an infectious disease. Though it’s obviously non-communicable, people with diabetes are more likely to develop intrinsic infections, such as gangrene (death of tissue caused by bacterial infection) and osteomyelitis (a type of bone infection), as well as extrinsic ones, such as tuberculosis (a bacterial infection that primarily attacks the lungs). People with diabetes also have worse outcomes when they catch an infection, as the COVID-19 pandemic showed, noted Gatete. Among patients hospitalized with severe COVID complications, just under 40% had diabetes.
“It’s clear diabetes and infectious disease are interconnected,” said Gatete. Meanwhile, heart disease is the leading cause of death for people with diabetes. These three conditions— diabetes, infectious disease, and heart disease—create a “triumvirate” that must be urgently addressed, said Gatete, who noted the IDF predicts a 134% increase in the total number of people with diabetes in sub-Saharan Africa by 2045. This would amount to 55 million Africans living with diabetes compared to 24 million today.
Achievement through partnership
Following Gatete’s presentation, which was part of the National Institute on Minority Health and Health Disparities (NIMHD) Seminar Series, Dr. Eliseo J. Pérez-Stable, director of NIMHD, noted that the research is “very practical. It could impact literally hundreds of thousands of people in Africa.” Yet he raised a key question: Once diagnosed, what do you do?
“The lifestyle intervention shown to be outstanding at preventing progression of pre-diabetes would be one way to start on a population basis as well as on a clinical basis,” said Pérez-Stable, who is co-lead of the NIMHD-NIDDK-Rwandan Health Program. “And what kind of pharmacotherapy would be accessible and inexpensive that could potentially be used for those most at risk?”
Dr. Tomlin Paul, a dean at University of Global Health Equity (UGHE) in Rwanda, echoed the concerns of Pérez-Stable. He stated, “diabetes is most devastating for LMICs as approximately 80% of the 463 million adults worldwide with diabetes live in low- and middle-income countries.” Yet only one in 10 people living with diabetes receives treatment recommended by WHO guidelines, he said. “Dr. Gatete’s research initiative is of great service to the cause.”
Paul concluded with praise for the Rwandan Health program, which provides one year of training at NIH to Rwandan physician-fellows and is also supported by UGHE and Partners in Health. “It is a novel learning collaborative. Graduates are already making significant contributions in the health sector.”
More Information
Updated June 14, 2023
To view Adobe PDF files,
download current, free accessible plug-ins from Adobe's website.
Related World Regions / Countries
Related Global Health Research Topics