Focus on suicide: Research boosts mental health task-shifting, innovative approaches
November / December 2018 | Volume 17, Number 6

Photo by Torsten Blackwood/AFP/Getty Images
Scientists in Fiji, which has one of the highest suicide rates in
the world, are studying task-shifting approaches to make up
for a shortage of psychiatrists.
By Karin Zeitvogel
Scant resources force low- and middle-income countries to use cost-conscious innovations to improve access to and standards of mental health care, with mobile technology and task-shifting often the tools of choice to achieve this.
A project supported by Fogarty and the National Institute of Mental Health (NIMH) in Bolivia is studying the use of mobile text messages to deliver cognitive behavioral therapy (CBT) messages to people with mental illness. CBT, which focuses on changing behavior that reinforces depression, has been shown to be more effective than antidepressants, explained Dr. John Piette of the University of Michigan, who’s leading the project. But accessing CBT usually requires several months of attendance at therapy sessions - not easy for people living on low incomes. “Putting CBT on people’s phones and using community health workers, who cost less than a psychiatrist, to monitor people’s health status makes care more accessible and less costly,” said Piette.
Similar approaches are also being studied in Fiji, said to have one of the highest suicide rates in the world. Researchers supported by Fogarty and NIMH are investigating how community health nurses, who have been trained to fill the gap created by a chronic shortage of psychiatrists, work with different diagnostic tools - a mobile phone questionnaire, a paper-based one, or the currently used system based on WHO guidelines. Initial results show the mobile phone app to be the most efficient at quickly providing caregivers with the critical information needed to flag people who are considering self-harm.
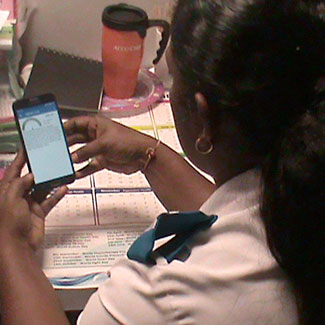
Photo courtesy of Dr. Vimla Patel
A community health nurse in Fiji uses a
mobile phone app to identify patients at risk
for suicide.
“Mobile technology appears to help nurses to rapidly and accurately identify people at risk for suicide,” said Dr. Vimla Patel, of the New York Academy of Medicine, and one of the principal investigators on the project. “We need to find at-risk people as early as possible to bring down Fiji’s high suicide rate.”
Mozambique began mental health task-shifting in the 1990s when it started training psychiatric technicians to compensate for a severe shortage of psychiatrists. Today, there are over 270 technicians countrywide, with at least one in every district. Although task-shifting has improved mental health care in Mozambique, access remains difficult in the country of 30 million, which is estimated to have the highest suicide rate in Africa.
With NIMH support, Dr. Bradley Wagenaar of the University of Washington (UW) is exploring ways to extend the reach of Mozambique’s overstretched mental health care providers. One project he’s working on allows patients to see - in a single visit to a clinic - a professional who can provide care for both physical and mental health problems. Called collaborative care, this approach has been found in U.S. trials to improve outcomes and lower costs for mental health patients. Part of the logic behind collaborative care is that mental illness, such as depression, is often linked to a patient’s chronic disease, said Wagenaar.
In another NIMH-supported project, Wagenaar is using something called the systems analysis and improvement approach (SAIA), which borrows elements from industrial engineering to chart the steps involved in the mental health care cascade, identify how patients and the health system are affected by them, and work with health workers to correct problems. Developed by UW researchers with NIH funding, this approach has already been used to improve outcomes in prevention of mother-to-child transmission of HIV.
SAIA was developed in Mozambique and is being tested and adapted for use in the U.S., said Wagenaar. The outcomes of the Fiji project are expected to guide the design of affordable, efficient systems that enhance health workers’ capacity to identify and treat depression and suicide risk, while protecting patient privacy.
“These are all examples of south-north flow of innovation,” said Wagenaar. “They illustrate how a two-way exchange of ideas helps to improve mental health care in underserved areas in low- and high-income countries.” And providing CBT by phone could help to improve access to non-pharmaceutical therapies both in LMICs and the U.S., where the suicide rate is high and growing.
More Information
To view Adobe PDF files,
download current, free accessible plug-ins from Adobe's website.