The Collaborative seeks to deepen interactions with policymakers, developing evidence based policy solution. This annotated bibliography provides a window into the literature on evidence-based policy and practice, as well as effective dissemination of scientific evidence:
- Theoretical frameworks for conceptualizing using evidence to inform policy.
- Practical tools for researchers and others seeking to move evidence forward to inform policy.
- Templates and examples of ways to communicate and disseminate research evidence and findings to diverse audiences in novel ways.
- Methods to reach government agencies and other decision-makers with new research findings in accessible and understandable means.
Theoretical Foundations and Frameworks
- Brownson, R. C., Chriqui, J. F., and Stamatakis, K. A. (2009)
Understanding evidence-based public health policy. American Journal of Public Health 99(9): 1576-1583.
Brownson et al describe three key domains of evidence based policy, process, content and outcomes. Engagement of all three streams is required to implement evidence-based policy, as well as to understand and document outcomes from policy change. The authors believe that application of these basic tenants is required to wisely invest limited government funding for health (Brownson, Chriqui, & Stamatakis, 2009). - Buekens, P., Keusch, G., Belizan, J., & Bhutta, Z. A. (2004).
Evidence-based global health. JAMA, 291(21), 2639-2641.
In this editorial the authors assert that the effectiveness of interventions being used to promote health in LMICs is untested. They argue that rather than a know-do gap, there is, in some cases, a lack of cluster randomized trials and observational studies to provide an evidence base for existing interventions already being implemented (Buekens, Keusch, Belizan, & Bhutta, 2004). - Campbell, D. M., Redman, S., Jorm, L., Cooke, M., Zwi, A. B., & Rychetnik, L. (2009).
Increasing the use of evidence in health policy: practice and views of policymakers and researchers. Australia and New Zealand Health Policy, 6(1), 21.
Authors examine the communication between researchers and policy makes to see how they work together and find that researchers do recognize the potential for evidence to contribute to policy. They find that four strategies are most successful supporting the contribution: 1) making findings understandable to policymakers, 2) increasing opportunities for interaction between policymakers and researchers, 3) addressing any structural barriers for research to link with policy like lack of incentives for academics, and lastly, 4) changing the research to make it more relevant to policy issues. - Harris, J. R., Cheadle, A., Hannon, P. A., Lichiello, P., Forehand, M., Mahoney, E., ... & Yarrow, J. (2012).
A framework for disseminating evidence-based health promotion practices. Preventing chronic disease, 9.
Harris and colleagues describe a framework for disseminating evidence-based health promotion developed at the University of Washington Health Promotions Research Center. They write that the key factors in dissemination are 1) a strong relationship between researchers and another organization that takes responsibility for the dissemination and 2) using principles from social marketing with potential end users. Relationships between the factors are visible in the Dissemination Framework Image, reproduced below in Figure 3.
Figure 3: Health Promotions Research Center
Dissemination Framework
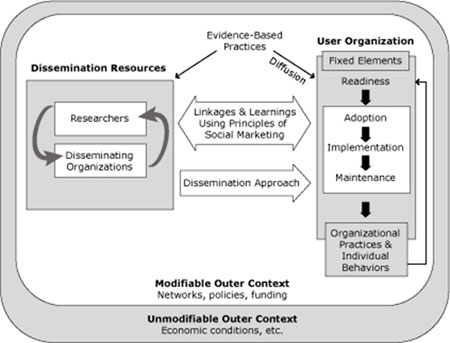
Source: Harris et al., 2012
Full description of
Figure 3: Health Promotions Research Center
Dissemination Framework:
Outer frame shows unmodifiable outer context, including economic conditions, etc. Inner
frame shows modifiable outer context, including networks, policies, funding. Within inner
framework: On left, dissemination resources (researchers and disseminating organizations).
On right, user organization shows flow among fixed elements (readiness, to adoption, to
implementation, to maintenance, to organizational practices and individual behaviors, which
points back to readiness). Evidence-based practices link dissemination resources and user
organization (with diffusion). Connecting left and right: linkages and learnings using principles
of social marketing flow both directions, dissemination approach flows just left to right.
Harris et al state, “The dissemination framework shows the resources (researchers and disseminating organizations) affecting a user organization through a dissemination approach developed collaboratively, using social marketing principles. The framework functions in an outer context of modifiable and unmodifiable elements (Harris et al., 2012; Padek et al., 2015). - Liverani, M., Hawkins, B., & Parkhurst, J. O. (2013).
Political and institutional influences on the use of evidence in public health policy. A systematic review. PLoS ONE 8(10): e77404.
Liverani and colleagues describe a body of literature that addresses the ways that the political nature of a given health issue might affect the use of relevant evidence, as well as whether and which government and institutional bureaucratic structures facilitate or impede use of evidence. Their conclusions is that awareness of the politics and institutional issues is important, and often not considered systematically (Liverani, Hawkins, & Parkhurst, 2013). - McCaughey, D., & Bruning, N. S. (2010).
Debate Rationality versus reality: the challenges of evidence-based decision making for health policy makers. Implementation Science 5(39).
Authors point out that policymakers are influenced by many factors in making decisions about health policy. Health policy does not necessarily maximize health outcomes based on evidence. Much of evidence-based medicine and evidence-based practice assumes a decision making process of individual rationality that we know is not true. Rationality assumptions of these models must be challenged to ensure that policy decisions are made effectively and consider the array of policy alternatives.
Tools for Communication
- Bardach, E. (2012).
Practical guide for policy analysis: the eightfold path to more effective problem solving 4th Ed. Los Angeles: Sage.
Bardach’s classic text describes eight practical steps framing a policy level problem, weighing the possible solutions, deciding on a policy, and framing the argument for that policy with a specific audience (Bardach, 2012). His eight steps include: 1) define the problem; 2) assemble some evidence; 3) construct the alternatives; 4) select the criteria; 5) project the outcomes; 6) confront the trade-offs; 7) decide; 8) tell your story. - Bennett, G., & Jessani, N. (Eds.). (2011).
The Knowledge Translation Toolkit: Bridging the Know-Do Gap, A Resource for Researchers. New Delhi, India: Sage Publications and International Development Research Centre.
Bennett and Jessani developed this Toolkit for the International Development Research Centre (IDRC) working with their counterpart in India. It offers tools for determining strategic approaches to audience identification and messaging, tips for key dissemination tools including news media, press releases, policy briefs, pamphlets, cartoons, online social networking, blogs, oral presentations, conference presentations, social media, and even community-level dissemination strategies like theatre and song. It also offers examples and templates for these tools. - Carpenter, D., Nieva, V., Albaghal, T., & Sorra, J., (2005) Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products). Rockville, MD: US Agency for Healthcare Research and Quality.
The US Agency for Health Research and Quality supported development of a very brief planning tool that walks though dissemination step by step visual guidance for thinking though dissemination, brainstorming audiences and thinking through the tools needed to reach those audiences. It is found within the edited volume based primarily on adapting E. M. Rogers' seminal Diffusion of Innovation Theory (Rogers, 1995). - Hovland, I. (2005).
Successful Communication: A Toolkit for Researchers and Civil Society Organizations. London: Overseas Development Institute.
Hovland offers planning tools for developing an overarching dissemination strategy for an intervention. Hovland details ways to best package a message and target it to audiences of interest. - International Development Research Centre. (2015).
How to Write a Policy Brief. Toolkit for Researchers. Canada: IRDC.
This tool was also developed by IDRC and is a simple, brief PowerPoint presentation and checklist with step by step instructions on presenting results appropriately and with maximum impact in the policy context. The last slide in this presentation contains a link to the IRDC checklist for developing a policy brief. - Schroeder, S. (2015).
Dissemination of Rural Health Research: A Toolkit. Grand Forks, ND: Rural Health Research and Policy Centers.
The authors explain that planning for dissemination is crucial. This document walks the user through the process of creating a strategy to get information to the people who need it, offering simple tips for effectual practice. Key guidelines on topics that may be important to the Learning Collaborative include: 1) effective titles increase the chances for an article to reach the right audience, including policymakers; 2) fact sheets need to be created with quick read formats for reaching policymakers; and 3) research summaries that frame research in terms of utility to a policy audience will provide policymakers with information that interests them. - Robinson, E., Baron, D., Heise, L., Moffett, J., & Harlan, S. (2011).
Communications Handbook for Clinical Trails: Strategies, Tips, and Tools to Manage Contraversy, Convey Your Message, and Disseminate Results. Family Health International: Washington DC.
This handbook offers plans and strategies to manage large scale communications plans that reach targeted audiences. It prioritizes engaging communities in dissemination before, during, and after a clinical trial. It also includes sample documents like brochures and contact lists for use as templates (Robinson, Baron, Heise, Moffett, & Harlan, 2011).
Works Cited
- Bardach, E. (2012). Practical guide for policy analysis: the eightfold path to more effective problem solving, 4th Ed. Los Angeles: Sage.
- Brownson, R. C., Chriqui, J. F., & Stamatakis, K. A. (2009). Understanding evidence-based public health policy. American journal of public health, 99(9), 1576-1583.
- Buekens, P., Keusch, G., Belizan, J., & Bhutta, Z. A. (2004). Evidence-based global health. JAMA, 291(21), 2639-2641.
- Harris, J., Cheadle, A., Hannon, P. A., Lichiello, P., Forehand, M., Mahoney, E., ... Yarrow, J. (2012). A framework for disseminating evidence-based health promotion practices. Preventing chronic disease, 9.
- Liverani, M., Hawkins, B., & Parkhurst, J. (2013). Political and institutional influences on the use of evidence in public health policy. A systematic review. PLoS One, 8(10), 1932-6203 (Electronic).
- Padek, M., Colditz, G., Dobbins, M., Koscielniak, N., Proctor, E. K., Sales, A. E., & Brownson, R. C. (2015). Developing educational competencies for dissemination and implementation research training programs: an exploratory analysis using card sorts. Implement Sci, 10(1), 114. doi: 10.1186/s13012-015-0304-3
- Robinson, E., Baron, D., Heise, L., Moffett, J., & Harlan, S. (2011). Communications Handbook for Clinical Trails: Strategies, Tips, and Tools to Manage Controversy, Convey Your Message, and Disseminate Results Retrieved from
http://www.fhi360.org/sites/default/files/media/documents/Communications%20Handbook%20for%20Clinical%20Trials.pdf
- Rogers, E. (1995). Diffusion of Innovations 4th Ed. New York, 15-23.
This toolkit is a product of and for the
Learning Collaborative for Implementation Science in Global Brain Disorders, which was initiated and is hosted by the Center for Global Health Studies at the Fogarty International Center, National Institutes of Health (NIH), and was developed in collaboration with members of the Learning Collaborative.
Partners in the Learning Collaborative include the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Institute of Mental Health (NIMH), the National Institute of Neurological Disorders and Stroke (NINDS), the National Institute on Aging (NIA), the Society of Neuroscientists of Africa (SONA), and the International Brain Research Organization (IBRO).
To view Adobe PDF files, download current, free accessible plug-ins from Adobe's website.